SPAIRE Hip - Preserving Muscles and Anatomy Enhancing Hip Stability and Recovery.
SPAIRE Hip
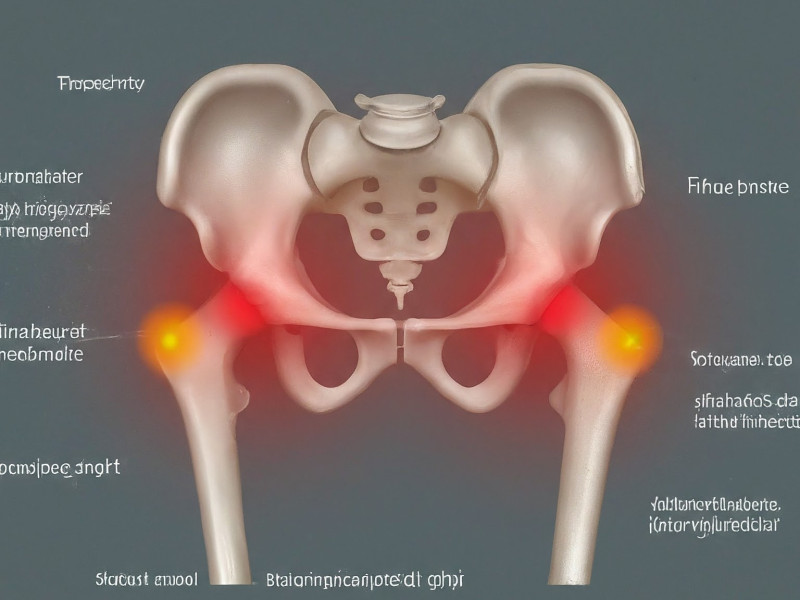
The SPAIRE (Soft-tissue Preserving, Anatomic, Internus muscle Retaining, External rotator preserving) technique is a muscle-sparing approach to hip replacement surgery. It aims to minimise postoperative pain, enhance hip stability, and improve functional outcomes by preserving the piriformis, obturator internus, and other short external rotators.
Key Benefits of SPAIRE
-
Muscle Preservation: By retaining the short external rotators and aiming to preserve the inferior gemellus, SPAIRE may facilitate improved hip stability, faster recovery, and potentially less postoperative pain.
-
Enhanced Postoperative Function: Research demonstrates that muscle-sparing approaches, such as SPAIRE, correlate with better gait and mobility after surgery (Charity et al., 2022; Lee et al., 2017; Selvaratnam et al., 2023). This includes quicker returns to daily activities and increased confidence in hip function.
-
Reduced Dislocation Risk: Preserving important stabilising structures reduces tension on the joint, potentially decreasing the risk of dislocation. When combined with modern technologies to further optimises stability.
-
Adaptability to Varied Cases: SPAIRE has shown success across different patient profiles, including high BMI and complex hip pathologies. Surgeons can selectively release tissues if necessary, retaining the option to address challenging anatomy without losing the main advantages of a posterior approach.
-
Potential for Less Pain and Fewer Complications: By limiting muscle trauma and preserving key anatomical structures, SPAIRE can help mitigate common sources of postoperative discomfort and mechanical instability.
Development of the SPAIRE Technique
The SPAIRE technique was developed in 2016 by Professor A. J. (John) Timperley and his team at Exeter. This work built on an understanding of the role of the short external rotator muscles in hip arthroplasty, and leveraged dedicated instruments and an offset introducer to facilitate optimal acetabular exposure.
-
Preservation of the Posterior Capsule: Instead of excising the posterior capsule, the capsule is repaired with an intra-osseous suture (the ‘RE’ part of SPAIRE).
-
Flexion & Abduction for Acetabular Exposure: The patient’s leg is placed on a Trimano support to help position the hip in flexion and abduction, yielding adequate exposure while minimising muscle trauma.
-
Scalability to All Cases: The SPAIRE technique has been successfully employed in patients of varying body habitus, including those with higher BMI. Professor Timperley has used it routinely for nine years, with only one early bail-out prior to the availability of specialised instruments.
-
Integration with Technology: Over the past seven years, SPAIRE has been combined with the MAKO robotic platform, further refining accuracy and clinical outcomes.
Distinction from External Rotator Preservation Procedure
Notably, when Professor Timperley developed SPAIRE, he had not yet encountered Kim’s work. Nevertheless, Kim’s study is acknowledged in the first SPAIRE publication (Hanly et al., 2017) for completeness. Professor Paul Lee, who trained alongside and was mentored by Professor Timperley in the SPAIRE technique, has been utilising it in his practice for many years. Together, they have published on the topic, further contributing to its body of evidence on SPAIRE’s development and history.
The External Rotator Preservation (ERP) procedure described by Kim et al. (2008) is sometimes confused with SPAIRE. However, Kim’s procedure differs significantly:
-
Complete Capsulectomy: Kim’s approach involved excising the posterior capsule. In contrast, SPAIRE repairs the capsule.
-
Positioning: Kim achieved exposure with flexion, adduction, and 90° internal rotation, reportedly leading to difficulties in controlling acetabular anteversion and retracting the femur.
-
Patient Selection: Kim et al. noted that ERP might not be suitable for higher BMI patients or certain pathologies. SPAIRE, however, has been demonstrated across a wide range of patients without limitation.
Notably, when Professor Timperley developed SPAIRE, he had not yet encountered Kim’s work. Nevertheless, Kim’s study is acknowledged in the first SPAIRE publication (Hanly et al., 2017) for completeness.
Biomechanical & Clinical Benefits
Muscle Preservation
By sparing the short external rotators (piriformis and obturator internus) and attempting to preserve the inferior gemellus, SPAIRE can support better postoperative stability, reduce soft-tissue disruption, and potentially aid in faster recovery.
Improved Stability & Mobility
Multiple studies have indicated improved hip stability and increased return to pre-injury levels of mobility with muscle-sparing methods. For instance:
-
Charity et al. (2022): Reported higher rates of returning to pre-injury mobility in patients who underwent SPAIRE hip hemiarthroplasty for displaced intracapsular hip fractures, compared to the standard lateral approach.
-
Selvaratnam et al. (2023): Found that SPAIRE was superior to the standard lateral approach for patients with a neck of femur fracture.
-
Lee et al. (2017): Documented early success with SPAIRE in hip surgery for various diagnoses.
Additional Perspectives from MSK Doctors
A dual mobility total hip replacement system, although not specifically part of SPAIRE, has been recommended for patients needing a greater range of motion before dislocation (Parikh et al., 2022). Similarly, studies examining short external rotator preservation suggest enhanced biomechanical outcomes and quicker recovery (Roger & Hill, 2012; Hanly et al., 2017). For further reading on these biomechanical advantages, see this study.
Summary
Although sometime there are confusions the SPAIRE technique is distinct from Kim’s External Rotator Preservation (ERP) approach and offers a robust, reproducible method for preserving key musculature in hip arthroplasty. Developed and described in detail by Professor John Timperley at Exeter, SPAIRE leverages a modified posterior interval, repairing rather than resecting the posterior capsule, using dedicated instrumentation, and allowing for broad applicability.

References:
Charity, J., Ball, S., & Timperley, A. (2022). The use of a modified posterior approach (spaire) may be associated with an increase in return to pre-injury level of mobility compared to a standard lateral approach in hemiarthroplasty for displaced intracapsular hip fractures: a single-centre study of the first 285 cases over a period of 3.5 years. European Journal of Trauma and Emergency Surgery, 49(1), 155-163. https://doi.org/10.1007/s00068-022-02047-1
Hanly, R., Sokolowski, S., & Timperley, A. (2017). The spaire technique allows sparing of the piriformis and obturator internus in a modified posterior approach to the hip. Hip International, 27(2), 205-209. https://doi.org/10.5301/hipint.5000490
Lee, P., Charity, J., & Timperley, J. (2017). Details of a tendon–sparing posterior approach in hemiarthroplasty in the treatment of displaced intracapsular neck of femur fracture. Journal of Arthritis, 06(03). https://doi.org/10.4172/2167-7921.1000243
Selvaratnam, V., Gunainthran, S., Akmal, I., & Kassim, A. (2023). The modified spare piriformis and internus, repair externus approach for hip arthroplasty. Cureus. https://doi.org/10.7759/cureus.34999
Kim, Yong Sik MD1,a; Kwon, Soon Yong MD2; Sun, Doo Hoon MD3; Han, Suk Ku MD4; Maloney, William J. MD5. Modified Posterior Approach to Total Hip Arthroplasty to Enhance Joint Stability. Clinical Orthopaedics and Related Research 466(2):p 294-299, February 2008. | DOI: 10.1007/s11999-007-0056-8






:format(webp)/cdn.mskdoctors.com/storage/profiles/2023/9/LbKKToiGARK3J2FwCeesxzv3EPmUdoE9.jpg)
:format(webp)/cdn.mskdoctors.com/storage/phBX64l1pEcTQ1HMDiT11FTt72xNeVN19uG2yYxA.png)
:format(webp)/cdn.mskdoctors.com/storage/QebHr80wQQ1HwgJHY2wYBKrh2xycCYuHWuKqSyR5.jpg)
:format(webp)/cdn.mskdoctors.com/storage/EeyugSe04aglm4G0BLfVCljZujwiXtbIQSjbFUc5.png)