Introduction to Medication Effects on Bone Density
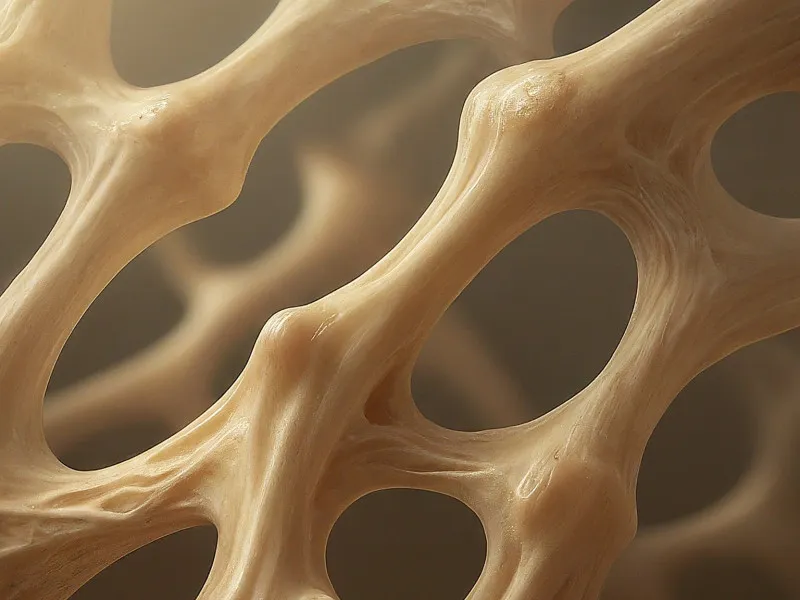
Bone density is a critical measure of bone strength, reflecting the concentration of minerals like calcium within the bone matrix. This parameter can be significantly influenced by various medications. In particular, long-term use of certain drugs can lead to decreased bone density, increasing the risk of osteoporosis. Understanding these effects and their mechanisms is essential for managing patient health effectively, especially in those requiring chronic medication therapy. Timely adjustments and preventive strategies can mitigate risks, fostering better long-term outcomes.
Medications Known to Affect Bone Density
Several classes of medications are known to influence bone density negatively. Glucocorticoids, often prescribed for inflammatory conditions, can inhibit bone formation and increase bone resorption, leading to osteoporosis with prolonged use. Antiepileptic drugs may alter vitamin D metabolism, negatively affecting bone mineralisation. Certain antiretrovirals and chemotherapeutic agents can also exert detrimental effects on bone health. While necessary for underlying conditions, these medications necessitate concurrent management strategies to protect bone integrity. Healthcare providers must assess bone health regularly and consider alternative treatments where feasible to minimise bone density degradation.
Clinical Management and Monitoring
Managing medication-induced changes in bone density requires a multifaceted approach. Regular monitoring through bone density scans can help detect early changes in bone health. Supplementation with calcium and vitamin D is often recommended to support bone metabolic needs, alongside lifestyle modifications such as increased physical activity and a healthy diet. In cases where significant bone density loss is detected, using medications like bisphosphonates to counteract resorptive processes may be necessary. Close collaboration between healthcare providers and patients ensures that medications for primary health conditions continue to provide benefits without compromising bone health significantly.
Emerging Treatments and Strategies
Advancements in medicine and research have ushered in new strategies for managing bone density issues associated with medication use. The development of selective cathepsin K inhibitors, such as odanacatib, shows promise in preserving bone mass while on long-term therapies. Additionally, new insights into the genetic interactions affecting bone density are paving the way for personalised medicine approaches, potentially allowing for tailored treatments that maximise efficacy while minimizing adverse impacts on bone health. Ongoing research continues to identify potential pharmacologic interventions aimed at maintaining bone density in patients reliant on long-term medication regimens.
When to Consult a Healthcare Provider
Patients should consult healthcare providers if they experience unexplained bone pain, frequent fractures, or other signs of deteriorating bone health while on medications. It is crucial for those at higher risk, such as postmenopausal women and older adults or those on long-term medication regimens, to undergo regular bone density assessments. Proactive dialogue with healthcare professionals ensures adequate monitoring, the timely introduction of protective treatments, and adjustments to medication regimens to mitigate impacts on bone health without compromising the primary treatment goals.
FAQs
What medications are known to affect bone density?
Glucocorticoids, antiepileptic drugs, antiretrovirals, and certain chemotherapy agents can negatively impact bone density, increasing osteoporosis risk with prolonged use.
How can I mitigate the effects of medications on my bone health?
Implementing dietary modifications rich in calcium and vitamin D, engaging in regular exercise, and undertaking routine bone density scans are effective strategies. Consult with your healthcare provider for tailored advice.
Are there medications that can help counteract bone loss?
Yes, medications such as bisphosphonates and newer agents like cathepsin K inhibitors can help maintain or increase bone density in patients experiencing medication-induced bone loss.
Should I stop my medication if I notice decreased bone density?
It is essential to consult your healthcare provider before making any changes to your medication regimen. There may be ways to protect bone health while continuing necessary therapy.
What are some emerging therapies for medication-induced bone density loss?
Selective cathepsin K inhibitors and genotypic assessments for personalised treatment plans are among the emerging innovations in addressing medication-induced bone loss.
How often should I get a bone density test if I am on medications affecting bone health?
The frequency of bone density tests will vary based on individual risk factors and the specific medications you are taking. Discuss an appropriate schedule with your healthcare provider.
References
- John A. Eisman et al., “Odanacatib in the Treatment of Postmenopausal Women with Low Bone Mineral Density: Three-Year Continued Therapy and Resolution of Effect,” Journal of Bone and Mineral Research.
- C. Ribot et al., “Bone Mineral Density and Thyroid Hormone Therapy,” Clinical Endocrinology.
- Richard D. Wasnich and Paul D. Miller, “Antifracture Efficacy of Antiresorptive Agents Are Related to Changes in Bone Density,” The Journal of Clinical Endocrinology & Metabolism.
